Learning from adverse events
About our shared learning to improve systems and minimise the possibility of future incidents.
On this page
Reporting serious adverse events
Reporting serious adverse events nationally is an important part of improving health outcomes for New Zealanders.
It improves safety and encourages open and transparent reporting of incidents when something goes wrong.
An adverse event is an incident which results in harm to people using health and disability services. Serious events are reported to the Health Quality & Safety Commission, in line with its national reportable events policy. Serious adverse events are generally those events where serious harm to a consumer or death has occurred.
The Learning from Adverse Event report is used to support our continuous quality improvement strategy, focusing on shared learning to improve systems and minimise the possibility of future incidents.
You can review our latest report below and/or see the hqsc.govt.nz for the national report.
Reports
The annual summary of adverse events data from 2019/20 has been released by the Health Quality & Safety Commission.
Each year, serious health care adverse events are reported to the Commission by district health boards (DHBs) and other health care providers. A serious adverse event is one that results in serious harm or death. The Commission works with providers to encourage an open culture of reporting, to learn from what happened, and to put in place systems to reduce the risk of recurrence.
Between 1 July 2019 and 30 June 2020, a total of 975 (916 in 2018/19) serious adverse events were reported to the Commission. Of these, 627 were reported by DHBs (566 in 2018/19). Clinical management events continue to make up the majority of reported adverse events. This includes pressure injuries, delayed diagnosis or treatment, deterioration, and complications.
Dr David Hughes, clinical lead for the Commission's adverse events programme, says that with lockdown and the ongoing COVID-19 response, this year has been extremely challenging for the health and disability sector.
'Now more than ever, we must remain focused on the quality of our care and on keeping our patients and ourselves safe.'
He says event numbers are closely linked to reporting rates, and an increase doesn't necessarily mean more adverse events have occurred.
'What it may in fact demonstrate is organisations continuing to develop an open culture where events are reported and learnt from, rather than an increase in preventable harm.'
Recently the Commission completed research into whānau Māori experiences of in-hospital adverse events, Ngā Taero a Kupe: Ngā wheako pānga kino ki ngā whānau Māori i rō hōhipera.
The research identified five major themes and two sub-themes from these experiences, including communication issues, perceived lack of care, lack of cultural safety and implicit bias.
Dr Hughes says that the insight gained from whānau Māori highlights the importance of putting the consumer and their families at the centre when responding to adverse events.
'These events are not just numbers. As health care providers, we have a responsibility to listen to the experiences of consumers and their whānau, learn from what went wrong and work to prevent harm to others.'
Key findings
Of the 975 reported adverse events:
- 627 were reported by DHBs
- 218 were reported from the mental health and addictions sector (DHBs only)
- 113 were reported by members of the NZ Private Surgical Hospitals Association (NZPSHA)
- 8 were reported by ambulance services
- 3 were reported from the primary sector
- 2 were reported from the aged care sector
- 2 were reported from a hospice
- 2 were reported by other providers
Of the 627 events reported by DHBs:
- 355 were clinical management events
- 231 were harm because of falls
- 20 were related to medication or IV fluid
- 13 were healthcare associated infections
- 4 were consumer accidents
- 3 were related to medical devices/equipment
- 1 was related to oxygen/gas vapour.
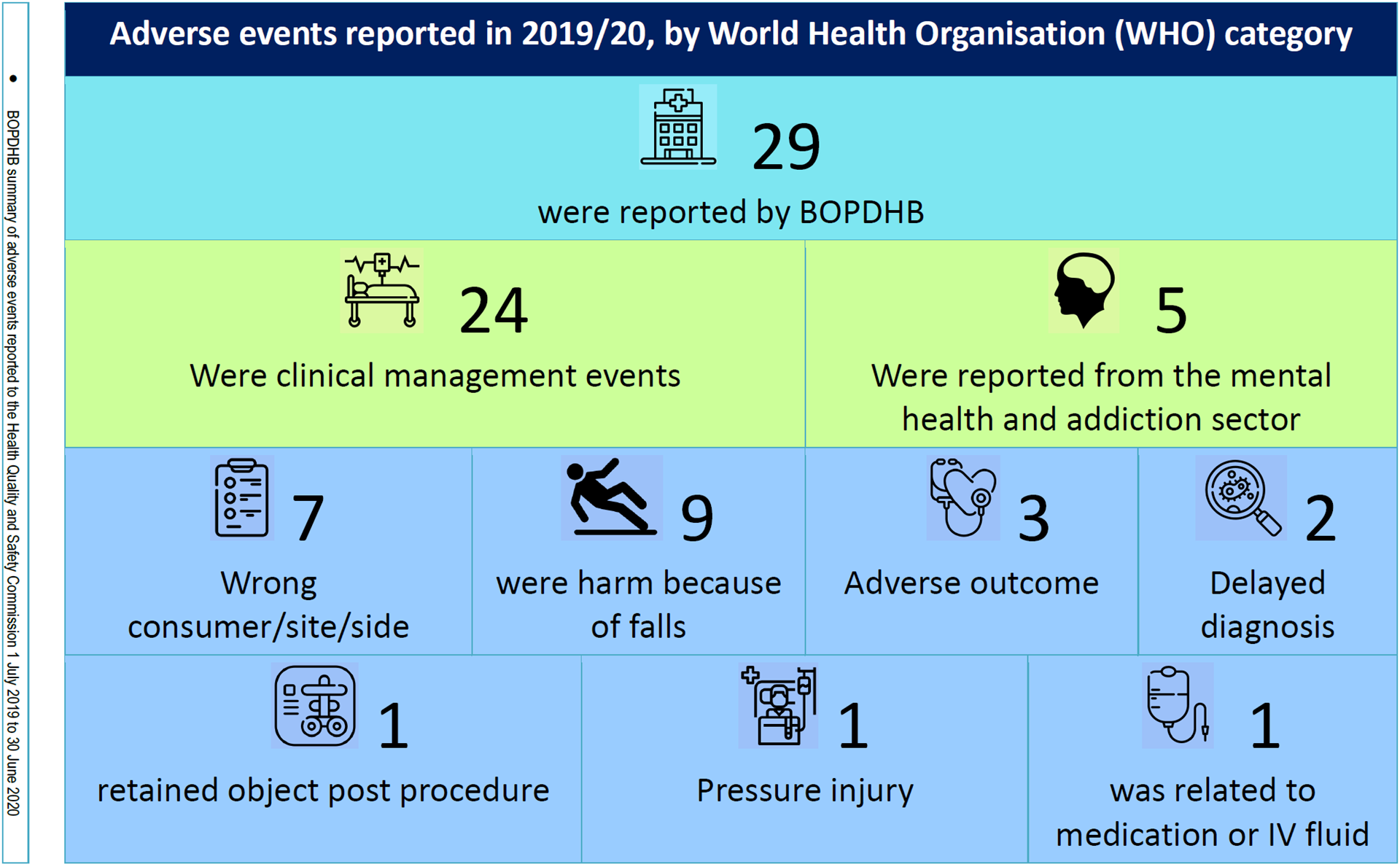
Below you will find information relating to adverse events reported at the BOPDHB during 2019/20.
BOPDHB adverse events reported in 2019/20 (by World Health Organisation category)
When a person has an adverse outcome as a result of their care with the BOPDHB we resolve to report the event, thoroughly review it and implement and any resulting recommendations, to ensure no other person and their family/whānau has the same experience.
Each year, health care adverse events are reported to the Commission by district health boards (DHBs) and other health care providers. The Commission works with these providers to encourage an open culture of reporting, to learn from what happened, and put in place systems to reduce the risk of recurrence.
Between 1 July 2018 and 30 June 2019, 916 adverse events were reported to the Commission. Clinical management events continue to make up the majority of reported adverse events.
Dr David Hughes, clinical lead for the Commission's adverse events programme, says the data in this report indicates that Māori are less likely to be reported as having had an adverse event.
'Of those events that have been reported, Māori are affected by adverse events where there is more scope for implicit bias to impact on their care, such as unrecognised deterioration.
'We are currently undertaking research into whānau Māori experiences of adverse events. We plan to use this research to develop recommendations for providers on how to better meet the needs of Māori who have experienced adverse events,' he says.
Total reported adverse events have fallen for the first time since 2011/12. Dr Hughes says in previous reports, the Commission has said that an increase in reported events does not necessarily mean an increase in harm. 'It is more likely to be as a result of better systems to identify existing harm. Equally, it would be unwise to say that a reduction in reported events is due to a reduction in harm.'
He says no one should experience preventable harm when they are recieving health care.
'The sector should work together to create a safety culture where people feel able to report harm without fear of being blamed for mistakes, and we can learn from what happened. We must do our best to prevent anyone else from being harmed.'
Key findings from all DHBs
Of the 916 reported adverse events:
- 566 were reported by DHBs
- 232 were reported from the mental health and addictions sector (DHBs only)
- 100 were reported by members of the NZ Private Surgical Hospitals Association
- 7 were reported by ambulance services
- 5 were reported from the primary sector
- 5 were reported by other providers
- 1 was reported from a hospice.
Of the 566 events reported by DHBs:
- 278 were clinical management events
- 255 were harm because of falls
- 18 were healthcare associated infections
- 11 were related to medication or IV fluid
- 1 was due to documentation
- 1 was related to nutrition
- 2 were consumer accidents.
All DHB figures
This table shows events reported annually by DHBs since 2015-2016. DHBs are steadily improving their reporting systems and more events are being reported and reviewed each year. It is not valid to compare the figures of different DHBs for a number of reasons, including widely varying population bases.
DHB adverse event numbers were correct at the time of data analysis for this report. There may be some variation in numbers included in this report compared with DHB data. This may relate to timing of reporting or reclassification following review.
|
DHB |
2015-16 |
2016-17 |
2017-18 |
2018-19 |
|---|---|---|---|---|
|
Northland |
17 |
21 |
19 |
18 |
|
Waitematā |
42 |
45 |
122 |
62 |
|
Auckland |
80 |
95 |
92 |
59 |
|
Counties Manukau |
58 |
48 |
42 |
38 |
|
Waikato |
41 |
44 |
49 |
62 |
|
Bay of Plenty |
9 |
14 |
13 |
25 |
|
Lakes |
11 |
13 |
13 |
6 |
|
Tairāwhiti |
8 |
6 |
6 |
10 |
|
Taranaki |
7 |
9 |
9 |
11 |
|
Whanganui |
17 |
9 |
1 |
13 |
|
Hawke's Bay |
13 |
21 |
24 |
25 |
|
MidCentral |
17 |
21 |
20 |
35 |
|
Hutt Valley |
7 |
6 |
15 |
13 |
|
Wairarapa |
3 |
8 |
7 |
3 |
|
Capital & Coast |
24 |
18 |
27 |
36 |
|
Nelson Marlborough |
41 |
9 |
8 |
6 |
|
West Coast |
8 |
9 |
8 |
4 |
|
Canterbury |
43 |
73 |
83 |
77 |
|
South Canterbury |
12 |
20 |
7 |
14 |
|
Southern |
62 |
53 |
66 |
49 |
BOPDHB Only Event Statistics
Note we are pleased with decreased number of Mental Health events
Adverse events
|
Event Type |
Number |
||
|---|---|---|---|
|
|
16/17 |
17/18 |
18/19 |
|
Clinical Management (including maternity) |
4 |
5 |
8 |
|
Healthcare Associated Infection |
4 |
0 |
2 |
|
Medication/IV Fluid |
0 |
0 |
3 |
|
Medical devices or equipment |
0 |
0 |
0 |
|
Consumer accidents |
0 |
0 |
0 |
|
Falls |
7 |
8 |
12 |
|
TOTAL |
15 |
13 |
25 |
Always report and review events
|
Event Type |
Total |
SAC 2 |
SAC 3 |
Sac 4/near miss |
|---|---|---|---|---|
|
Wrong blood component |
0 |
0 |
0 |
0 |
|
Retained foreign object post - procedure |
1 |
0 |
0 |
1 |
|
Wrong site, wrong implant/prosthesis, wrong consumer/procedure |
5 |
0 |
5 |
5 |
Mental Health Adverse Events
|
Type of event |
Community |
Inpatient |
Total |
|---|---|---|---|
|
Suspected Suicide |
5 |
0 |
5 |
|
Serious Self Harm |
0 |
0 |
0 |
|
Serious Adverse Behaviour |
0 |
0 |
0 |
|
TOTAL |
5 |
0 |
5 |
When a person has an adverse outcome as a result of their care with the BOPDHB we resolve to report the event, thoroughly review it and implement any resulting recommendations, to ensure no other person and their family/whanau has the same experience.
In 2017/2018, 631 people nationally had an adverse outcome which met the criteria for reporting to the Health Quality and Safety Commission (HQSC).This is an increase on previous years and is likely due to changes in requirements for reporting along with better reporting within DHBs.
However, even with increased reporting the serious adverse events numbers at the BOPDHB for 2017/18 have come down from 2016/17.
Learning from Adverse Events | 1 July 2017 to 30 June 2018 | What are the individual DHB figures? This table shows events reported annually by DHBs since 2015-2016. DHBs are steadily improving their reporting systems and more events are being reported and reviewed each year. It is not valid to compare the figures of different DHBs for a number of reasons, including widely varying population bases.
DHB adverse event numbers were correct at the time of data analysis for this report. There may be some variation in numbers included in this report compared with DHB data. This may relate to timing of reporting or reclassification following review.
|
DHB |
2015-16 |
2016-17 |
2017-18 |
|---|---|---|---|
|
Northland |
17 |
21 |
19 |
|
Waitemata |
42 |
45 |
122 |
|
Auckland |
80 |
95 |
92 |
|
Counties Manukau |
58 |
48 |
42 |
|
Waikato |
41 |
44 |
49 |
|
Bay of Plenty |
9 |
14 |
13 |
|
Lakes |
11 |
13 |
14 |
|
Tairāwhiti |
8 |
6 |
5 |
|
Taranaki |
7 |
9 |
9 |
|
Whanganui |
17 |
9 |
1 |
|
Hawke's Bay |
13 |
21 |
24 |
|
MidCentral |
17 |
21 |
20 |
|
Hutt Valley |
7 |
6 |
15 |
|
Wairarapa |
3 |
8 |
7 |
|
Capital & Coast |
24 |
18 |
27 |
|
Nelson Marlborough |
41 |
9 |
7 |
|
West Coast |
8 |
9 |
8 |
|
Canterbury |
43 |
73 |
83 |
|
South Canterbury |
12 |
20 |
8 |
|
Otago |
|
|
|
|
Southland |
|
|
|
|
Southern |
62 |
53 |
66 |
This year also represents the first time since 2013 that mental health and addiction service events have been included in the Adverse Events reporting.
Adverse events
|
Event Type |
Number |
|
|---|---|---|
|
|
16/17 |
17/18 |
|
Clinical Management |
4 |
5 |
|
Healthcare Associated Infection |
4 |
0 |
|
Medication/IV Fluid |
0 |
0 |
|
Medical devices or equipment |
0 |
0 |
|
Consumer accidents |
0 |
0 |
|
Falls |
7 |
8 |
|
TOTAL |
15 |
13 |
Always report and review events
|
Event Type |
Total |
SAC 2 |
SAC 3 |
Sac 4/ |
|---|---|---|---|---|
|
Wrong blood component |
0 |
0 |
0 |
0 |
|
Retained foreign object post - procedure |
3 |
0 |
1 |
2 |
|
Wrong site, wrong implant/prosthesis, wrong consumer/procedure |
4 |
0 |
2 |
2 |
Mental Health Adverse Events
|
Type of event |
Community |
Inpatient |
Total |
|---|---|---|---|
|
Suspected Suicide |
13 |
1 |
14 |
|
Serious Self Harm |
0 |
1 |
1 |
|
Serious Adverse Behaviour |
0 |
0 |
0 |
|
TOTAL |
13 |
2 |
15 |
Adverse Events (excluding mental health events) reported to Health Quality & Safety Commission (HQSC)
|
Description of Event |
Review Findings |
Recommendations/Actions |
Follow Up |
|---|---|---|---|
|
Harm from Falls: Falls in hospital have a huge impact on the patient and their family/whanau. The work that has been undertaken has shown improvement against the HQSC outcome measure.
|
|||
|
Inpatient fall resulting in death due to subdural haematoma |
Elderly patient who had a falls risk assessment completed and care plan in place. Despite being supervised patient fell while dressing after a shower and struck head causing a subdural haematoma.
Patient very unwell on admission. On review the fall, which was an unfortunate accident, was deemed a contributing factor in the patient's death. |
NIL |
NIL |
|
Inpatient fall resulting in death due to subdural haemorrhage |
Elderly patient, who was extremely unwell due to multiple comorbidities, assessed as high falls risk. Falls prevention strategies implemented unclear if invisibeam activated.
Unwitnessed fall. |
Need to ensure the invisibeam is positioned accurately to pick up patient movement. |
Ongoing education regarding placement of invisibeams. |
|
Inpatient fall resulting in fractured hip |
Elderly patient with history of involuntary movements and other comorbidities fell when trying to get up.
Plan - to assist patient to mobilise, nonslip socks, call bell within reach (not activated by patient for assistance) - was in place. Patient also positioned in room close to nurses' station and rounded/checked 20/30mins prior to fall. |
Requirements for assessing and documenting falls risk assessment subject to ongoing education and training. |
Ongoing |
|
Inpatient fall resulting in fractured ankle |
Elderly patient assessed as a high falls risk due to cognitive impairment and general weakness. Required assistance with mobilising, attempted to mobilise without assistance and fell.
Unwitnessed fall. |
All high risk patients with cognitive impairment to have an ultra-low bed and full head-to-toe assessment following a fall. |
Ongoing |
|
Inpatient fall resulting in fractured hip |
Elderly patient with multiple comorbidities assessed as high falls risk and plan of care identified which included using a walking frame to mobilise.
Patient had been allocated a walking frame but refused to use it.
Unwitnessed fall. |
NIL |
NIL |
|
Inpatient fall resulting in fractured hip
|
Elderly patient assessed as falls risk and an appropriate plan of care implemented. Patient was very unwell and had been fully assessed 20 minutes prior to the incident.
Unwitnessed fall. |
NIL |
NIL |
|
Inpatient fall resulting in fractured hip
|
Elderly patient with complex behaviours was assessed and identified as a high falls risk. Despite a comprehensive plan of care in place the patient had an unwitnessed fall during the night. |
NIL |
NIL |
|
Surgical Site Infections - SSI (Deep) - Met the criteria for reporting as part of ongoing surveillance of SSI. BOPDHB like other DHBs has not previously reported these events but chose to start reporting as it is a key indicator of patient safety. |
|||
|
Surgical site infection following hip replacement
|
Patient underwent an elective hip replacement, two months post original surgery diagnosed with deep infection at site resulting in further surgery. Reviewed at service mortality and morbidity meeting; no actions identified which could have prevented this. |
NIL |
NIL |
|
Surgical site infection following hip replacement |
Patient had to return to theatre for washout of hip following total hip replacement two weeks prior.
Patient had significant risk factors for infection. |
Ongoing auditing of SSI and compliance with quality and safety markers. |
Ongoing |
|
Surgical site infection following hip replacement |
Patient underwent total hip joint replacement with uncomplicated recovery. Readmitted three weeks post-surgery with infection requiring return to surgery for wash out.
Procedure followed best practice. No issues found with theatre environment.
Patient was nursed in four-bedded room post-surgery; on day two new admission into the room with hip cellulitis. |
Increased emphasis on hand hygiene and vigilance on patient placement in the surgical ward.
Ongoing auditing of SSI and compliance with quality and safety markers. |
Ongoing |
|
Surgical site infection following hip replacement |
Patient readmitted with deep surgical site infection 17 days post total hip joint replacement.
Multiple risk factors which contributed to infection. No breach in procedures identified. |
Ongoing auditing of SSI and compliance with quality and safety markers. |
Ongoing |
|
Clinical events |
|||
|
Unexpected outcome following surgery |
Patient admitted with severe sepsis, from a complex abscess in the neck. Surgery was indicated and appropriate. The operation was long and complex requiring extensive neck flexion.
This was high risk surgery and even if neck flexion had been kept to a minimum paralysis could still occur as an unexpected complication. Permanent paralysis. |
Share the learnings to highlight the need to be aware of the possibility of spinal stenosis in patients undergoing complex neck surgery. |
Actioned |
|
Delayed treatment resulting in heart damage |
Patient left the department without staff being aware, returned the next day in a worse condition, resulting in unnecessary harm.
Due to a lack of signals in the system when the patient initially presented they were not identified and managed as a GP referral resulting in delays in care.
The demand and capability of department was extreme and required a crisis response. |
Systems and processes in the department reviewed and updated to mitigate the possibility of a similar event.
|
The learnings from this event informed changes in the department and issues addressed. |
|
Wrong patient received MRI |
Patient received MRI intended for another patient.
Two referrals for two different patients with the same name and similar age were received by radiology one was for an MRI and the other a CT. |
Process reviewed referrals for patients with the same name are not to be processed together. |
Staff reminded of care required when processing referrals for patients with the same name. |
Learning from Adverse Events (excluding mental health events) reported to Health Quality & Safety Commission
|
Description of Event |
Review Findings |
Recommendations/ |
Follow Up |
|---|---|---|---|
|
Inpatient fall resulting in fractured NOF
|
Elderly patient with dementia had a restless night, getting up and down, and on this occasion slipped. Patient was assessed as being at risk of falls on admission and was wearing non-slip socks and incontinence products but the risk assessment had not been updated to reflect current needs. |
Risk assessments need to be regularly reviewed and updated in line with changes in clinical presentation and treatment plans updated accordingly.
Consider trial of an Invisi beam to see if this would be sturdier and the client is not able to step over this. |
Requirements for risk assessment and care planning are ongoing.
Invisi beams were trialled but not deemed appropriate. A bell mat for each bed space in the mental health older person's ward have subsequently been purchased. |
|
Inpatient fall resulting in fractured leg (Femur)
|
Unwitnessed fall. Falls risk assessment and careplan completed and reflective of current requirements. Patient had a history of dementia and was being supported in hospital by family who stayed overnight. At time of the fall staff were unaware that family had left. |
The DHB has a care capacity demand management programme which includes variance response management, this is reviewed regularly and strategies put in place to meet demand. |
Ongoing |
|
Inpatient fall resulting in fractured ribs |
Patient admitted with fractured hip and was recovering in rehabilitation ward. Was identified as at high risk of falls, falls careplan in place and was wearing appropriate non-slip footwear at the time. |
Nil |
Nil |
|
Inpatient fall resulting in fractured leg (Femur)
|
Elderly patient assessed as at high risk of falls, requiring assistance when mobilising. Was mobilising with walking frame to the bathroom with assistance from a family member and staff. Patient had sudden collapse, fall broken by people assisting. |
Nil. |
Nil |
|
Inpatient fall resulting in fractured pelvis
|
Elderly patient went to toilet without calling for assistance and had an unwitnessed fall resulting in fractured pelvis. Patient stated had been to the toilet, turned to shut door and fell.
Assessed as being at high risk of falls, requiring assistance when mobilising and invisi beam in place. Patient went to toilet without calling for assistance, no footwear on and invisi beam found to be off as result of earlier intervention. |
Reminders to staff, to be vigilant with patients who have invisi and ensure they are switched on as part of the "rounding" check.
Patients who are at high risk of falls and may suffer cognitive lapses should wear non slip socks in bed as well as having slippers by the bed. |
Nil |
|
Inpatient fall resulting in fractured knee
|
Patient had been assessed as at risk of falls and plan was for them to be assisted to the bathroom. On this occasion the call bell was within reach, however the patient decided to attempt mobilising independently with frame. As patient got out of bed and attempted to move with frame they fell, landing on their knees. |
Nil |
Nil |
|
Inpatient fall resulting in fractured hip
|
Patient mobilising from x-ray slide to own bed. Nurse sat patient on the side of the bed and placed the walker in front of them. The nurse was organising the patient's IDC, IV lines, machines and monitors etc. when the patient suddenly fell forwards into the frame which slipped underneath them and they fell on the floor.
|
Learning outcome: prepare the patient for stages of mobilisation (communicate each step prior). Plan to talk the patient through each step and assess patient ability to physically perform the next step. RN to keep one hand free to steady the patient if required. |
Ongoing |
|
Wrong site surgery - incorrect skin lesion removed
|
The correct leg was marked but not the lesion. This was picked up during a check once the patient was anesthetised. Efforts were made to identify the likely lesion for removal and an agreement reached and surgery proceeded. Subsequently found the wrong lesion removed.
|
Review Surgical Safety Checklist Protocol and work with the Perioperative Improving Surgical Safety Team to ensure requirements for marking of skin lesions is explicit.
In cases where there is uncertainty the surgery must not proceed. |
Ongoing |
|
Mode of surgery not consented to.
|
Patient booked for a hysterectomy was expecting the procedure to be performed as a total laparoscopic hysterectomy (TLH) but surgery performed as a total abdominal hysterectomy (TAH).
Reasons for this were that there were two different Notices for Admission (NFA) for the same patient, one for TLH and one for TAH.
The consent section of the form for the procedure was mistakenly sighted as having been correctly signed during the pre-operative 'Sign-In' check.
The omission was noted when the patient was anesthetised prior to surgery but the decision was made to proceed without the proper signed consent. |
|
Completed - no further issues since. Current foci for this national programme are:
|
Serious Adverse Events (excluding mental health events) reported to Health Quality & Safety Commission
|
Description of Event |
Review Findings |
Recommendations/ |
Follow Up |
|---|---|---|---|
|
Inpatient fall resulting in fractured hip
|
Patient recalled sitting on the side of the bed and then being on the floor, thought their leg "just gave way".
No documented falls risk assessment. Despite this the risk of falls for this patient was identified and appropriate plan of care in place for mobilising.
|
Falls programme includes strategies to improve compliance with QSMs (quality and safety markers).
Intentional rounding includes checks of environment |
Nil |
|
Inpatient fall resulting in three fractures
|
Patient with history of osteoarthritis, who usually mobilised with walking frame and one person assist, was sitting up on the edge of bed. Patient got up and transferred to the lazy boy chair without assistance.
Patient had bare feet, this combined with the vinyl fabric of the lazy boy, which is a slippery surface, appears to have resulted in the patient falling. Fractures treated with conservative management. |
Patient careplan should have included use of appropriate footwear which includes non-slip socks.
Falls programme includes availability of double sided non slip socks. |
Nil |
|
Inpatient fall resulting in fractured ribs
|
Unwitnessed fall. Patient complaining of pain stated they had a fall earlier in the bathroom and was assisted off the floor by someone in blue. Nobody could corroborate this.
Difficult to establish how fractured ribs were sustained.
Patient assessed as high falls risk with plan in place - mobilise with assistance, nurse in single room on low low bed with sensor mat. |
Nil |
Nil |
|
Inpatient fall resulting in fractured collar bone
|
Falls risk assessment completed and documented had identified patient as high risk, history of previous fractures from falls. Discussed having bed rails up as enabler but patient declined this.
Patient in contact isolation. Had been getting intermittent confusion but was last observed sleeping. Patient explained they were reaching out of bed for Lotto scratch cards which had fallen on the floor and they tumbled out. |
Nil |
Nil |
|
Inpatient fall resulting in fractured hip
|
Unwitnessed fall. Patient with multiple comorbidities including postural hypotension, elements of dementia with increased periods of confusion. Initial assessment identified patient as high risk of falls and needing assistance with mobility no further documented assessment ot plan of care following transfer to a ward. Family member present and willing to stay to ensure patient had constant supervision. Staff encouraged family member to go home indicating patient would receive the level of care they needed.
No evidence of nursing care plan completion although response to risk of falls documented on TrendCare handover sheets. |
Falls programme includes strategies to improve compliance with QSMs.
Ongoing education regarding patient and family centred care and support persons. |
Ongoing communication with the family member caring for this patient they presented their story to BOPDHB board and the story is used in ongoing education particularly around aspect of support person role and welcoming them to stay. |
|
Inpatient fall resulting in fractured hip
|
Elderly patient with severe osteoarthritis and poor mobility assessed as high falls risk. Plan of care included patient being nursed on a low low bed to assist with transfer and at night, as it was this night it was positioned on its lowest point. Staff went to assist another person in the room during the night and found patient out of their bed and lying on the floor next to the bed.
This patients' comorbidity made them an extremely high risk of fracture. |
Nil |
Nil |
|
Inpatient fall resulting in fractured hip
|
Patient was in communal lounge area mobilising independently and was walking past another client who was suffering from a condition causing involuntary movements and was knocked resulting in the patient losing their balance and falling to the ground.
Whilst in some aspects this was an unforeseen incident due to the unpredictability of both clients it does highlight the already identified hazards with the environment. |
Environment not conducive to needs of clients who require wide spaces to manage behaviour.
Risk assessments need to be regularly reviewed and updated. |
Ongoing The environment is an identified hazard which is managed and monitored through the hazard register. Regular audits of risk assessment . |
|
Inpatient fall resulting in fractured pelvis
|
Assessed as able to mobilise with walking frame and assistance. Taken to bathroom by nurse, towels on floor from previous patient whilst nurse picking these up patient fell. |
Principles of intentional rounding environment checks to be extended to all areas including bathrooms. |
Ongoing |
|
Inpatient fall resulting subdural haematoma
|
Patient with multiple comorbidities including a history of falls at home and previous brain bleeds had a fall resulting in new bleed.
Falls risk assessment completed and care plan documented, noting patient required assistance with mobilising. Patient appears to have got up unassisted to go to the toilet and fallen. |
Nil |
Nil |
|
Inpatient fall resulting fractured pelvis
|
Frail patient with multiple comorbidities including osteoporosis. Falls risk assessment completed and careplan was walk with 1 x assistance and frame, requires assistance with sitting on the toilet and hygiene cares and safe transfer from toilet to stand.
Nursing staff assisted patient onto the toilet advising them to ring call bell when finished and left them unattended in the bathroom, for patient's privacy. Patient reports they thought they could manage to get off the toilet by themselves so did not use call bell. |
The need to supervise patients that require it at all times included in ongoing education. |
Ongoing |
|
Inpatient fall resulting fractured hip
|
Elderly patient who had a documented falls risk assessment. High falls risk due to recent falls at home, able to mobilise with stick and assistance x1 from staff. Seen by staff five minutes prior to fall, no confusion and did not require assistance with anything. Patient subsequently mobilised independently to toilet without requesting assistance and fell fracturing hip below prosthesis. |
Nil |
Nil |
|
Inpatient fall resulting fractured hip
|
Patient assessed as falls risk and requiring assistance rang the call bell but before it was answered, got up and used their walking frame. Whilst attempting to open the toilet door patient fell.
Contributing factors staff availability during meal breaks, size, weight and structure of bathroom door.
|
The importance of ensuring colleagues are aware of when staff take breaks so they can respond to call bells in absences.
The doors meet required standards but are an identified hazard for frail elderly. |
Included in ongoing education. |
|
Query removal of BIPAP (Bilevel Positive Airway Pressure) contributed to patient death
|
The patient was significantly compromised on arrival to hospital and their death as a result of their medical state was not unexpected. The review was undertaken due to concerns with management of BIPAP.
No HDU (High Dependency Unit) bed available initially, placed in APU (Admissions Planning Unit) and later transferred to ward, no evidence of re referral to HDU.
|
A number of recommendations were made in regard to:
|
Subject to ongoing coroner and HDC investigation. |
Actions taken in response to falls
We have a falls prevention programme which is continually monitored and reviewed to ensure best-practice is applied to reduce harm.
There are two falls working groups. One reviews the organisational Reportable Event Forms (REFs) related to a fall and the second monitors what is happening nationally, regionally and locally.
Some examples of outcomes from these groups are:
- changes to floor mopping processes and associated education
- ongoing education emphasising the need for reassessment of falls risk care plan when patient mental status changes
- ward unit level work adopting a bottom-up approach giving individual wards ownership of the programme
- intentional rounding including environmental checks, ensuring that aids are within reach
- non-slip socks standardised to having grips all round the foot with improved fit.
The falls prevention programme focuses on fall risk assessment and care planning. Compliance is monitored through quality and safety markers (QSM).
Improving documentation is a focus area.
Quality Accounts
Our patients are at the very heart of everything we do.
We work hard to continually improve our health service by collaborating with our staff, patients, family, whānau, carers and community.
Our quality account reports demonstrate our commitment to providing safe high-quality healthcare, show how we monitor quality and safety, and describe how changes are made as part of a continuous quality improvement approach for our population.
