For health professionals
For health professionals
On this page
- Informational videos
- Connect with other clinicians
- Training links
- Clinicians' resources
- Legal terms
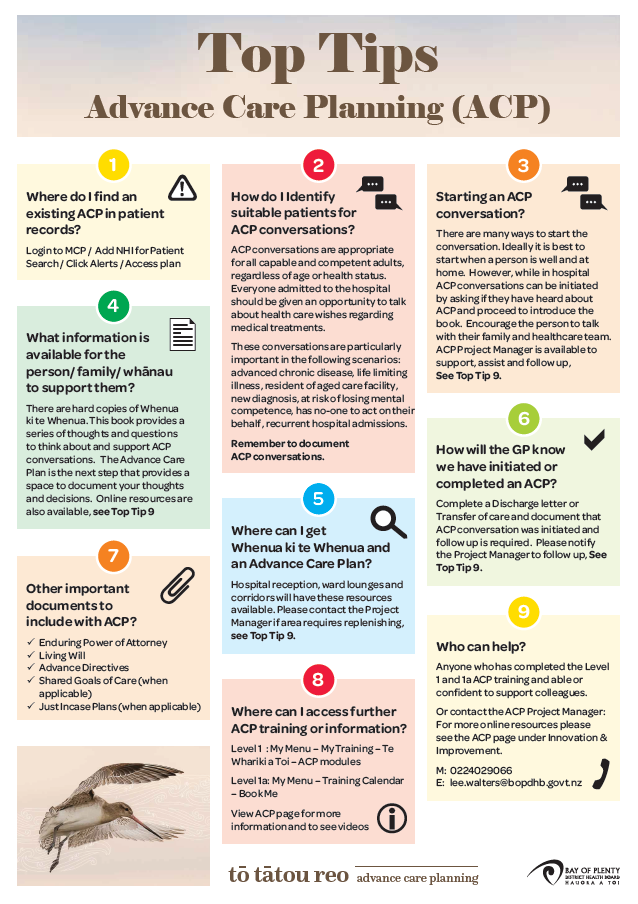
- ACP Top Tips resource poster
Informational videos
An Overview of Advanced Care Planning in New Zealand
In New Zealand, advance care planning is a process. The focus is on understanding what is important now and in the future. This video gives an overview of the advance care planning process including the tools available to support this work.
Primary Care Nurse Practitioner Julia Perry speaks about the benefits of having an Advance Care Plan
Connect with other clinicians
Connect with other professionals at the Advance Care Planning (ACP) Facebook page. This site is monitored by HQSC Health Quality & Safety Commission.
Training links
Get links to training here: https://tewharikiatoi.ac.nz/login/index.php
- Te whāriki o Toi: Level 1a ACP (*training calendar)
- Level 1 ACP modules
- Assisted Dying Mods
- Shared Goals of Care
Note: To access all online learning modules (ie Level 1, assisted dying, etc) please use the same link.
Clinicians' resources
 The HQSC Shared Goals of Care Plan contains information about recognising and responding to acute deterioration and the importance of having shared goals of care discussions with patients and their whānau.
The HQSC Shared Goals of Care Plan contains information about recognising and responding to acute deterioration and the importance of having shared goals of care discussions with patients and their whānau.
Download the shared goals of care case for change
Find additional resources and get the HQSC Shared Goals of Care guide.
Check with your colleagues to see if they have any experience with Advance Care Planning. About 70 people in the Bay of Plenty have completed the ACP training so far and are dotted around the organisation.
A good place to start is HQSC's Advance Care Planning (ACP) webpage. Here you can complete the online self-assessment and then try the introductory modules.
There are also a couple of tools that may be useful. The first is the Serious Illness Conversation Guide that comes from Ariadne Labs in the United States of America. It's a series of eight questions that have been tested on patients and can help get the information you want.
Atul Gawande (author of Being Mortal) has refined the questions even further and created Five Questions:
- What is your understanding of where you are and of your illness?
- Your fears or worries for the future?
- Your goals and priorities?
- What outcomes are unacceptable to you? What are you willing to sacrifice and not?
And later, - What would a good day look like?
The libraries at both Tauranga and Whakatāne hospitals have books about this as well.
 The Aotearoa serious illness conversation guide forms part of the Commission's serious illness conversation programme, supported by district health boards.
The Aotearoa serious illness conversation guide forms part of the Commission's serious illness conversation programme, supported by district health boards.
The guide is a set of structured questions to help clinicians who do not come from a palliative care background, have conversations with seriously ill people and their whānau about what is most important to them if time were limited and/or their functional abilities were to change.
Download the Aotearoa serious illness conversation guide
Find comprehensive resources for serious illness discussions at the HQSC website
The Aotearoa drill sheet to support serious conversations is part of the Commission's serious illness conversation programme, supported by district health boards.
Download the drill sheet to support serious illness conversations
Find comprehensive resources for serious illness discussions at the HQSC website
 'Just in Case’ plans aim to improve the experience and outcomes of palliative and end-of-life patients by developing a plan around their future needs, wishes and quality of life considerations.
'Just in Case’ plans aim to improve the experience and outcomes of palliative and end-of-life patients by developing a plan around their future needs, wishes and quality of life considerations.
This patient-held plan can be referred to by whānau and caregivers, and used by other healthcare providers to enable a more integrated and seamless approach to palliative care closer to home.
The objective is to increase the provision of primary palliative care in the community through proactive plans and improved service integration, and reduce hospital transfers whenever possible and appropriate.
Just in Case plans should be developed between the patient and a clinician who knows them well, such as with the GP or their NP. However, hospital clinicians can develop a temporary plan to facilitate this right care process, and request for the GP or NP to review and countersign or change the plan within two weeks.
 Medical Care Guidance to support the development of a parallel process to ACP for patients who permanently lack capacity.
Medical Care Guidance to support the development of a parallel process to ACP for patients who permanently lack capacity.
Legal terms
This video is designed to help clinicians understand the legal framework of advance care planning including enduring powers of attorney for personal care and welfare and advance directives.
ACP Top Tips resource poster